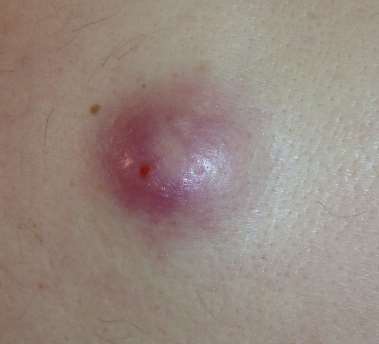
What is an abcess?
An abscess is a collection of pus. Pus is a fluid consisting of SERUM (from the blood), dead and destroyed body cells, bacteria (both dead and alive), sometimes blood and other products of tissue destruction.
Whenever an abscess occurs, there has been tissue destruction. This is often caused by bacteria which invade the body through cuts, punctures, and after surgery. Some abscesses form in special areas and are associated with adjacent problems; eg dental abscesses usually mean caries or gum disease. Sometimes they form without any recognized injury. Abscesses can form in virtually any part of the body.
Are abcesses dangerous?
Potentially yes. All abscesses can cause serious harm if left alone or not properly treated, especially in diabetics. While small abscesses may settle without medical treatment, larger ones can spread to involve adjacent organs or invade the blood stream (septicemia).

How are they treated?
Treatment aims to drain the pus. This often involves making a small cut (incision) over the abscess. In special locations and situations a needlemay be used to drain the pus away without cutting.With large abcesses, the cavity left after releasing the pus may need to be packed for several days before the abcess can heal. Packing allows healthy tissue to replace the infected walls of the cavity. If this is not done, there is every chance that pus will reform.
Can an abscess come back?
Yes. An abscess may form at any time in virtually any area of the body. Even after surgery, pus may re-accummulate at the original location.
Is surgery for this condition dangerous?
More often, it is more dangerous NOT to have surgery. Even a very old or ill person is usually made dramatically better by draining an abscess. Small abscesses are usually drained in the office but larger ones often require general anaesthesia (being put to sleep) which increases the risk of surgery, especially in infants or the elderly.
And after the operation?
Some locations heal rapidly after an abscess is drained. Other times, the area may need to be packed and dressed for several days to ensure good healing, especially in large or deep- seated abscesses.
Will I be normal after surgery?
After all is healed you will be normal in the vast majority of cases. Some abscesses (in bone) may lead to deformity, but this is fortunately not often. Really major abscesses, such as those in internal organs like the brain or liver can however lead to severe disability, including death. In diabetics an abscess in the foot may lead to amputation and the disability this causes. Happily most abscesses occur just under or in the skin and though painful are usually trivial.
How soon can I go back to work?
In most cases abscesses heal in a week to 10 days. Complicated or large ones may take several weeks to fully heal. Your doctor will make sure you're cured before allowing you back to work.

What is an amputation?
This is the removal of a limb, or part of a limb. Most commonly, it is the lower limb that is involved, but the upper limb may also become so infected or gangrenous after major injuries as to render amputation necessary.
Why do I need it?
The most common reason for amputation is GANGRENE of a part of the limb. This refers to the death of tissue. This condition is most commonly seen in diabetics and hypertensives whose circulation is so poor that tissues in the foot die. This may occur after an injury, but may also happen without apparent injury.
Is it a dangerous condition?
Every effort will usually have been made to preserve your limb, but if gangrene sets in, and cannot be stopped, removal of the affected part of the limb may be the only way to save your life or relieve your pain. Untreated, gangrene can quickly lead to further death of tissue, and loss of life by massive infection, called septicemia.
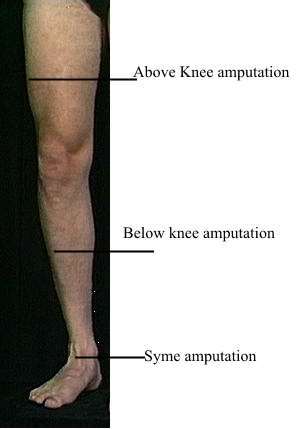
What will surgery do?
Remove part of the limb. In the lower limb, there are only a few levels where an amputation is performed (see diagram). These are a) above the knee; b) below the knee; c) occasionally across the instep; d) at the level of the toes.
Can it come back again?
Gangrene may occur again, either in the same limb or the other. The causes will usually be similar - poor circulation. This is why it is essential to look after the feet carefully, especially if you have already had an amputation, or suffer from poor circulation
Is surgery for this condition dangerous?
Not usually. Occasionally gangrene may be so advanced that toxicity ("blood poisoning") may be present. This will increase the danger of surgery; but it also makes it more imperative to have the surgery to prevent further toxicity - which may lead to death.
In the very elderly, or if your general state has been seriously affected by diabetes, the risks of surgery will increase.

What about after the operation?
Loss of a limb is always tragic, since it always affects one's function and enjoyment of life. Prostheses (artificial limbs) are available for every kind of amputation. These dramatically improve life, and can make the difference between having to depend on others, and being totally independent. In some cases you may need to make minor adjustments to your house - such as ramps, safety handles in bathrooms etc - to make getting around a bit easier. In some cases, you may even be able to continue driving a car after an amputation
Can I work after the operation?
Yes, provided you are given the okay by your doctor. If you have been provided with a prosthesis, you may even return to a perfectly normal lifestyle, with minor changes.
Can I function normally again?
Rehabilitation may involve PHYSIOTHERAPY to get your muscular strength and balance back to normal. After you have regained your normal poise, and your stump has healed, you should be able to enjoy a relatively happy life, especially if you have a well fitted prosthesis
Can I prevent it?
It is sadly often the case that many amputations in diabetics and other people with poor circulation can be prevented. Usually the injuries that lead to limb loss appear trivial at the beginning - a little "scrape", a small nail "juk" or a "simple" bruise can lead to fast spreading infection that can threaten the health of the entire limb. As long as you have diabetes or poor circulation, you should resist the urge to treat these "simple" conditions yourself. Seeing your doctor early is the best way to prevent an amputation.
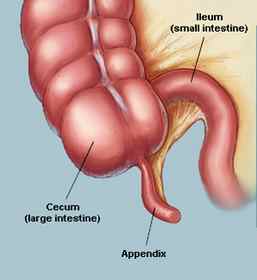
What is appendicitis?
This is removal of the appendix. The appendix is a small closed tube of bowel attached to the first part of the large bowel, called the cecum. This normally lies in the right lower abdomen. Most often the appendix is removed when is inflamed - acute appendicitis.
How did I get it?
The appendix may become inflamed when pellets of stool block the lumen (inside), causing the tip to become swollen and inflamed. At other times, there may be no observable cause, though there is evidence that this condition is in some way related to one's diet. "Modern" diets appear to predispose to appendicitis more so than "primitive" diets rich in natural foods.
Is it a dangerous condition?
Usually the pain of acute appendicitis will bring a person to a doctor quickly enough for treatment to be given early. If treatment is unduly delayed, appendicitis can become a grave condition, and even today may cause death. Delay can lead to abcess formation or rupture of the swollen appendix, a very serious condition in many cases.
What will surgery do?
Remove the infected appendix through a small incision (cut) in the right lower abdomen under a general anaesthetic. The diseased organ is then submitted for pathological study to confirm the diagnosis.
Can it come back again?
No. After the appendix is removed, you will not have any further attacks of appendicitis.
Is surgery for this condition dangerous?
Not usually. However, it is well to remind you that any general anaesthetic may lead to complications. If you have any underlying medical conditions such as diabetes or high blood pressure, these may increase the usually small risk of the operation.
What about after the operation?
You will usually be home in one to two days, and should be your normal self in about a week. If there has been a lot of pus, as can happen if an appendix ruptures, then your hospital stay will be longer. Very occasionally a really bad case of appendicitis can lead to long hospitalization and several operations, but this is rare. You can live quite happily without the appendix.
Can I work after the operation?
Certainly, after complete recovery.
Can I function normally again?
Yes, in every way. The appendix is not required for normal functioning of the body. Its loss will not be noticed in any way.
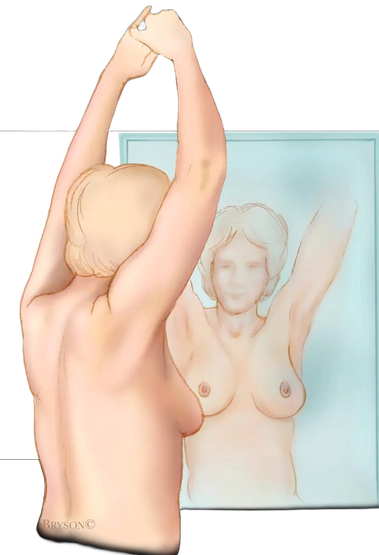
Breast self-palpation
Breast cancer can be cured completely in a number of cases if it is detected early enough. This is the reason for the emphasis that is being placed on self-palpation of the breast by women in general.
Knowing your breast
One would think that since all women "know" their breasts that they are aware when lumps form. In actual fact, the majority of women are often the last to appreciate disease occurring in their own breasts. Many women do not make it a practice to examine their breasts; those that do often do it inadequately; while others do not know what to feel for. The following presents a simple guide in the hope that you will become more adept at what could be a life saving procedure.
The Method
1) This begins with an inspection of the breasts, preferably standing in front a mirror. You should note:
- the size of the breasts - is one breast larger than the other?
- the nipples - do they stand out normally?
- Sudden retraction (where the nipple disappears into the breast tissue) may indicate serious disease.
- Is there any unusual unevenness in the contour or shape?
- Are there any rash or sores on the nipple or areola?
- Is there a discharge from the nipple?
- Is there any change in skin texture in any part of the breast? A thickening of the skin with prominent pores (looking like an orange skin) is a serious sign.
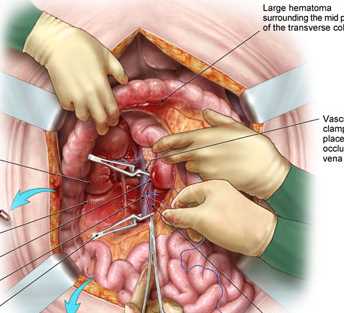
What is a laparotomy?
This is the medical term applied to opening the abdominal cavity. It is not a specific operation per se, and is often used when the precise nature of the surgery needed cannot be determined before an inspection of the abdominal organs is done.
Why do I need it?
A laparotomy is often indicated when there is abdominal pain of uncertain origin, or when there is a lump (mass) in the abdomen. An emergency laparotomy is often required in stab or gunshot injuries to the abdomen. At other times, abnormalities can occur without pain or a mass, which may still demand surgery.
Is the operation dangerous?
A laparotomy is classified as major surgery because (with very few exceptions indeed) it has to be done under general anaesthesia. While opening the abdomen and merely doing an inspection is very simple, remember that further surgery is often required. It is the nature of this further surgery which may increase the overall risks.
What will surgery do?
Under general anaesthesia (you will be put to sleep), an incision (cut) is made in the front of the abdomen, and the abdominal cavity is opened. This allows all of the abdominal organs like the liver, intestine, pancreas, spleen, stomach, gallbladder, etc to be seen or felt directly. If any disease process is identified, then further surgery may be done on any of these organs. Sometimes, despite previous pain or other symptoms, all organs appear completely normal on inspection. In this case, nothing further is done, except that the appendix may be removed so as to avoid the possibility of a future appendicitis.
Is this surgery dangerous?
All major surgery carries some risks, including a (very small) risk of death. A laparotomy per se has very little risk attached to it, but if further surgery is needed, other risk factors enter the picture. Do remember that diabetes, hypertension, heart disease, obesity and advanced age all increase the general risks for all surgery. If you are fit and healthy, the risks are all less.
There is one general complication from laparotomy for any reason. During the healing process bands of tissue called ADHESIONS may form. These generally are silent and do not cause trouble ever. In a few cases though, adhesions may result in acute obstruction of the small bowel. If this does not subside on its own, further surgery may be needed to cut these bands and allow normal bowel function. Obviously, even this operation (to remove adhesions), may itself cause further adhesions .....
What about after the operation?
Provided that minimal (or no) surgery was done, recovery from a laparotomy is quick and complete. You will have a scar on the abdomen, but provided that you do not suffer from cheloids, this heals well. If there has been major surgery, then you will be informed in this regard by your doctor as soon as you recover sufficiently.
Can I work again after this operation?
After healing of the wound and of any internal organs that may have been operated on is complete, you will usually be completely well and able to resume normal work. There will be a period of medical leave to allow you to readjust to normal life and its demands.
Will I function normally again?
After complete convalescence, yes. If specific surgical procedures have been done which involve any changes in your life-style, your doctor will discuss these with you.
Special comments.
Remember that a laparotomy is often done for conditions about which one is not certain. This makes it difficult for you to give consent for specific surgical operations. The final choice about what to do must often be left to the surgeon after he/she inspects the abdominal organs.
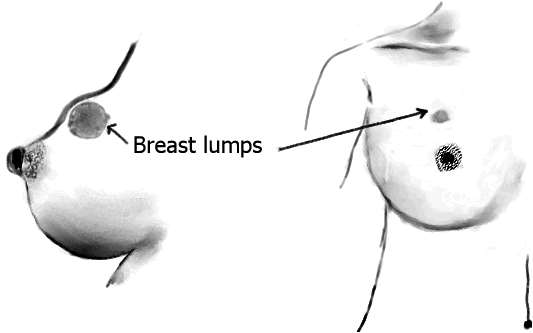
What is a breast lump?
Any swelling in the breast is a breast lump. The vast majority of these are BENIGN (ie not cancer), but since this assessment can never be made for sure without a pathological report, most lumps are BIOPSIED (see below). Lumps can be solid, or may contain fluid (cysts). Often what is thought to be a lump is really an area of lumpy breast tissue, not a true lump.
How did I get it?
Breast lumps can develop at any age. The cause for these lumps is not known for certain. During puberty, pregnancy and while breast-feeding, the breasts of many females may feel lumpy, but often do not contain true lumps. As a general rule, anytime a lump is felt or suspected, you should check with your doctor. This is especially true if a member of your family has had previous breast problems, notably cancer.
Is it a dangerous condition?
In the majority of cases, a breast lump is a benign (non-cancerous) condition. However, any lump in the breast should be considered potentially dangerous until checked and diagnosed by a doctor. He or she may needle the lump, perform a BIOPSY, or at least keep the lump under observation for some time.
What will surgery do?
The term BIOPSY is applied to the usual surgery for lumps in the breast. This involves removing either the entire lump (excision biopsy) or a part of it (incision biopsy) for the pathologist to study. This procedure is usually done under local anaesthesia and takes a few minutes. It may also be done with a special needle introduced through the skin.
Can it come back again?
Yes. Lumps can form in the breast at any time in the life of a female (or indeed a male). If this happens, check your doctor again.
Is surgery for this condition dangerous?
Not in the least. Provided you are in good health, it is a simple and safe procedure often done in the office or outpatient theatre. Large lumps, or malignant lumps may require more extensive surgery which may need general anaesthesia in hospital.
What about after the operation?
Except for some mild soreness at the site of the operation, you should have no ill effects. The sutures (if any) are usually removed in 5 to 7 days.
Can I work after the operation?
You will be perfectly normal after about a week, unless you are informed otherwise.
Can I function normally again?
Yes. A biopsy in no way affects the normal function of the breast. Breast feeding in later pregnancies should not be affected in any way. After surgery it is common for local hardness to be felt at the site of the surgery. This is part of normal healing, and will usually gradually disappear in 2 to 3 months.
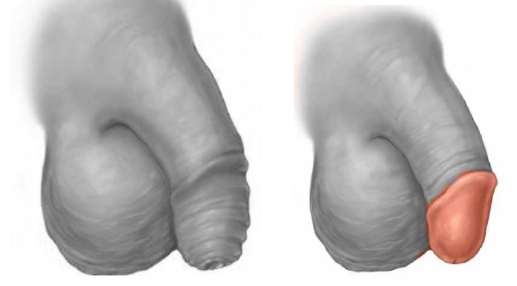
What is a circumcision?
This is removal of the foreskin, or prepuce - the loose jacket of skin covering the tip of the penis. Many cases of circumcision are done for religious or cultural reasons, as in Muslims and Jews. Some also do it for personal reasons. But many cases are required for medical reasons, as outlined below. Recent data has shown that it can reduce the male susceptibility to HIV infection.
Why do I need it?
Circumcision is performed for a number of problems. The usual one is PHIMOSIS, when the foreskin is too tight to allow normal hygiene and/or sexual activity. In this case, troublesome cracks often occur. Very occasionally trauma or acute infection may also be a cause.
Not usually. However, if a previously normal foreskin suddenly becomes difficult to go back, it may conceal potentially dangerous conditions affecting the penis, some of which may lead to cancer. For this reason, any phimosis in an adult male should be seen and investigated by a doctor.
What will surgery do?
Remove the last inch or so of the foreskin. This will leave the tip of the penis (the GLANS) exposed.
Can the foreskin give trouble again?
Usually no, since it no longer exists.
Is surgery for this condition dangerous?
Surgery is performed under local anaesthesia for adults, and general anaesthesia for small children. The dangers under local anaesthesia are minimal - indeed almost unknown. Perhaps the most troublesome is bleeding which can appear frightening at times. In order to lessen the risk of this, you should obey the instructions given you, especially resting for the first two to three days, and of course avoiding sexual activity. For children, the main potential for danger lies in the anaesthetic.
What about after the operation?
After a circumcision, the area just behind the tip of THE PENIS WILL SWELL. It will look horrible (to you) and in adults will be uncomfortable. To minimise these difficulties, it is important (esp. for adults) to lie down and rest for the first three days. Children generally will have few problems. Though it may not appear so, the penis will return completely to normal.
You need not worry about the sutures; these will dissolve in about 10 to 14 days.
Can I work after the operation?
You will need about a week to 10 days before returning to work.
Can I function normally again?
Yes. After a variable time of between 3 to 6 weeks, the penis will be completely normal once more. A circumcision in no way endangers your sexual ability once healing is complete. You should allow at least 4 to 6 weeks before restarting normal sexual activity.

What is a MASTECTOMY?
The term MASTECTOMY refers to the removal of the breast. This operation is seldom performed for any other cause except cancer of the breast. Happily, with early detection of breast cancers when they are relatively early and small, many cases that would otherwise have required removal of the entire breast can now be treated with local resection (removal) of the lump WITHOUT remoing the whole breast. This is a major advance in treatment over the past.
How did I get cancer of the breast?
The cause for this condition is not entirely known in all cases. As far as we know, it is not related to anything you have or haven't done DIRECTLY. We do know, however, that breast cancer is more common in persons who have other members of their family similarly affected, as well as in women who have never had children. There are also lifestyle decisions that appear to increase the chances of breast cancer, like smoking and being obese. It may also occur in men.
Is it a dangerous condition?
Yes, unfortunately. That is why you have been advised to have the breast removed. By so doing, we hope to remove all the cancerous tissue, and so minimize future complications. If the cancer is found at an early stage when it is still small, it is usually possible to remove only the lump, leaving the breast for cosmetic reasons.
What will surgery do?
You will be put to sleep (general anaesthesia), and the breast tissue will be removed from the chest wall. The skin will be closed with sutures (stitches). You may find a long tube coming from under the skin. This is a drain which merely helps remove fluid and post-operative bleeding from the area. If only the lump is to be removed, the rest of the breast will of course be left in place.
Can it come back again?
This is possible. For this reason, you will be kept under observation for the rest of your life, at increasingly longer periods. From time to time you may undergo Xrays, ultrasounds and blood tests to determine if there any signs of recurrence.
Is surgery for this condition dangerous?
Not really, provided you are generally fit. Small breasts are naturally easier to remove than large ones. Remember, any major operation may lead to unexpected complications. However, this operation is usually well tolerated in healthy people.

What about after the operation?
The major concern of most women is that removal of the breast will leave them flat-chested on one side
This is true, but there are many options open for cosmetic correction. However, this is usually a later concern. Stitches are usually removed in about 7 to 10 days. You should eat normally. Be very careful not to inadvertently pull out the drain, should you be discharged from hospital with it in place.
You may also be advised to have further therapy, usually in the form of radiation and / or chemotherapy. This is to further minimize the possible late effects of cancer cells which may have escaped from the breast and spread to adjacent areas. These can lie dormant only to start growing again years later.
Can I work after the operation?
Yes. When all is healed, you will lead a normal productive life again.
Can I function normally again?
Yes. This is a serious disease, but with good and speedy medical care, many women soon return to their normal activities. For those who desire it, prosthetic surgery is available to reconstruct a normal looking breast using either implantable devices under the skin (silicone or saline filled) or natural fat and muscle tissue taken from the abdomen, chest wall or back.
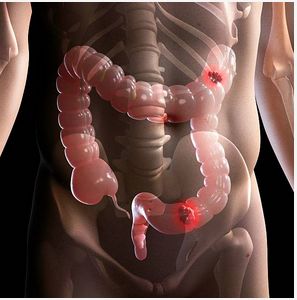
What is a colectomy?
A colectomy is the removal of the colon. Usually this is not a true colectomy, but a hemi-colectomy - that is, removal of part of the colon. Right hemi-colectomy refers to removal of the right half of the colon.
Why do I need it?
Because this part of the bowel is severely diseased in some way. A decision has been made that leaving the colon (or the malfunctioning part of it) behind, would lead to serious ill-health.
Is the condition that I have dangerous?
The need for a colectomy or hemicolectomy is always serious. Your doctor will have explained the full details to you already. In general removal of the colon is done most often for the following major diseases:
- cancer of the bowel
- advanced diverticulitis which has caused complications like bleeding, infection or abcess formation.
- life-threatening ulcerative colitis
- major trauma to the bowel- as in gunshot injuries etc
What will surgery do?
Under general anaesthesia, the abdomen is opened, an inspection is made to determine the extent of the problem, and the appropriate part of the large bowel is then removed. Every effort is then made to rejoin the bowel so that normal toilet function returns. In some cases, however, this is not possible and a colostomy may have to be performed. A colostomy is an opening on the front of the abdomen through which stool is discharged. It may be temporary, but sometimes is permanent.
Can the condition come back again?
This all depends on what precisely is the problem. You should discuss this with your doctor. In general most conditions for which this operation is done can recur in later years in another part of the bowel.
Is surgery for this condition dangerous?
A colectomy is major surgery. As such there are risks that you should be aware of. Many complications are possible, both during and after the operation. If you are hypertensive, diabetic, asthmatic or very elderly, all the risks increase.
Infection is one of the most serious complications. Bleeding during surgery can usually be controlled, but may also occur after surgery. A breakdown of the suture line in the bowel is a life-threatening event, but happily is not common. It is common for the alimentary tract to be in a state of ileus after surgery, during which it does not work normally. You will not be able to eat or drink during this period. Occasionally this may proceed to frank obstruction, and may require further surgery.
Other general complications include pneumonia, and deep vein thrombosis, especially in persons who are obese or elderly.
What about after the operation?
Convalescence after colectomy is generally reasonably long, and most persons can expect to be in hospital for one to two weeks. By this time, the bowel should have begun to return to normal.
Can I work again after this operation?
Certainly, provided all goes well. In the main, you can expect to be on medical leave for at least a month to six weeks, in some cases more.
Will I function normally again?
This depends on several factors, the most significant being whether there was a need for a colostomy. If normal bowel continuity has been achieved, you can expect to function normally. A colostomy will require a significant amount of getting used to, but the vast majority of individuals learn to manage perfectly well in time.
Special comments.
It is especially important that you discuss all these factors with your doctor before agreeing to colectomy. Be sure you fully understand what is involved and any significant changes to your life style post-operatively.
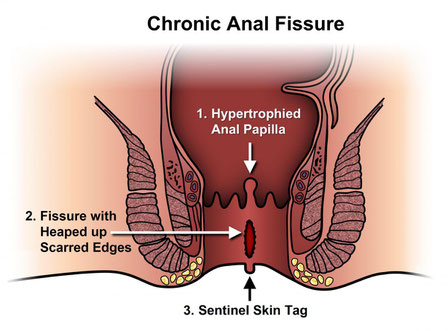
What is a fissure?
The full name for this condition is fissure-in-ano (literally a crack or tear in the anus). It is not to be confused with the similar-sounding, but quite different, fistula-in-ano.
How did I get it?
The skin of the anal canal is really quite thin and easily torn. A fissure commonly results when one is constipated. Passage of the hard mass of stool, especially when this occurs explosively attended by severe straining, can tear the lining of the lower anal canal, creating a fissure-in-ano. If there are sharp objects in the stool (such as bones), it is possible for these to lacerate the anus. Fissures may also form when the large bowel is inflamed.
Is the condition dangerous?
Not dangerous, but it can be very painful indeed. This is because the anus is extremely well supplied by nerve fibres, making it very sensitive. These fissures in reality are often quite small and insignificant in appearance, but can cause excruciating discomfort at stool. This is most likely to occur if the person continues to be constipated, which is often.
The reason for this is that pain in or near the anus tends to inhibit the very desire to stool. Feces then accumulates in the rectum, becoming harder with each passing day. When this is finally passed as another hard, constipated stool, it compounds the situation by further irritating the fissure.
How is the condition treated?
First by using measures to relieve the pain and discomfort in the anus. Various creams and suppositories which contain local anaesthetics are often recommended, and can assist tremendously. As you would imagine, the most urgent need is to correct the cause of the fissure - that is constipation. Most persons who have this condition typically do not take enough fibre in their diet. Fibre can be had by eating more vegetables (not over-cooked) and fruit. But in this condition there are a number of fibre preparations which are prescribed for more rapid relief.
With these measures, most fissures heal in about two to three weeks. Some however may last for months, and may even require surgery to assist in healing.
It is often recommended to have a complete assessment of the lower bowel after the acute pain subsides. This may mean having a sigmoidoscopy, colonoscopy or barium enema. The aim of these examinations is to rule out the presence of other disease entities which may mimic or cause a fissure in ano.
Can it come back again?
Of course it can. Not a few persons who have fissures cured revert to their previous low fibre diets, only to become constipated again.
Is surgery for this condition dangerous?
Surgery for fissure in ano is usually a last resort after healing has failed to occur on its own. It is not by any means dangerous, and involves excising the old fissure which by now usually consists of a mass of chronically inflamed, fibrotic tissue. The new wound often heals well, provided that constipation can be avoided.
What about after the operation?
Pain and constipation are the main problems post-operatively. Pain relieving medication coupled with sea (or Sitz) baths and adequate rest from work in combination are usual treatment methods.
Can I work again after this operation?
After healing is complete, yes. But you will almost certainly require some time from work to allow for complete healing.
Will I function normally again?
Happily all fissures eventually heal, provided they are not associated with any other serious disorders. After healing you will be completely normal. But remember - stick to a high fibre diet and adequate fluids. This will ensure that your bowel motions are regular and even enjoyable!!
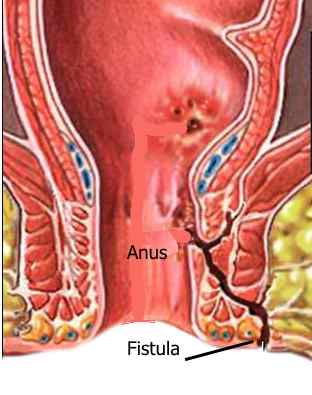
What is a fistula-in-ano?
This is an opening adjacent to the anus which generally oozes small quantities of bloody fluid or pus. Sometimes it occurs after an abcess has been drained around the anus. At other times, it appears without warning.
How did I get it?
The opening you can see next to the anus is really only part of a more complex problem. A fistula is really a tract that burrows from the skin, through the tissues around the anus to enter the lower anal canal. Through this tract small amounts of infected material pass from the anus, eventually discharging through the opening. It is because of this persistent connection with the anal canal that few fistulae can close without surgery. Some fistulae can be caused by inflammatory conditions in the rectum, like ulcerative colitis.
Is a fistula dangerous?
In itself, not really. There is little or no danger to life itself. However the constant oozing of pus, swelling, occasional pain, and general discomfort make this condition a real nuisance. Occasionally, an abcess may form, requiring emergency surgery.
Can it be cured?
In the majority of cases, yes. But this requires surgery. Sometimes a fistula seems to disappear on its own, but this is very uncommon.
What will surgery do?
The aim of surgery is to completely excise the fistula, including the opening as well as the tract. This leaves a defect next to the anus which has be dressed until it heals. This sort of surgery has to be done under a general anaesthetic.
What about after the operation?
or the first few days you will experience some local discomfort at the operative site, and may need to remain in hospital until the acute pain settles. After this you will be discharged, but will need to attend hospital or the office every day for dressings. This unfortunately will have to continue until complete healing, which may take three weeks or longer. Daily sea baths help considerably to lessen the pain and discomfort. You will naturally be given analgesics (pain killers).
Will I function normally again?
Stooling will be a bit painful for the first week, but gradually improves. You will also find difficulty sitting for long periods. However with time and patience all these difficulties will gradually improve as the ulcer heals.
Can a fistula come back again?
It certainly can. This may be because it only appeared to heal but was not completely cured. In these situations it is not unusual to find that when you least expect, the opening reappears. On the other hand a completely new fistula may occur in anyone at any time, if the conditions are right. This is especially true if you have inflammatory bowel disease.
So what can I do to avoid a recurrence?
Not a lot really. About the most important would be to inform your doctor at once if you feel any discomfort or niggling pain around the anus after having a previous fistula operated on. Other than this you should observe the rules of good health and hygiene. Specifically it would be recommended to maintain a high fibre diet. If you have inflammatory bowel disease, keep in contact with your physician. And do your best to avoid a promiscuous life style; some STD's (sexually transmitted diseases) can cause fistulae to form.
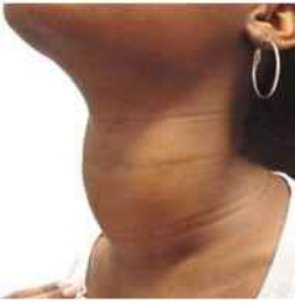
What is a goitre?
A goitre is an enlarged thyroid gland. The thyroid is a gland that is situated in the front of the neck, and is responsible for regulating the metabolic rate (that is, the general activity level) of the body.
How did I get it?
A wide variety of causes exist - including puberty, pregnancy, some medications, and abnormalities in the way the body handles iodine. The gland may also be swollen because of cysts. Cancer too may be a cause of an enlarged thyroid. In many cases the precise cause is not known for certain.
Is it a dangerous condition?
This depends on the cause. An overactive thyroid gland (thyrotoxicosis) can lead to a number of serious problems including weight loss, heart failure, bulging eyes, menstrual irregularities. Cancer too will lead to further problems if not managed speedily. If the gland is large because of cysts, then it poses little danger.
What will surgery do?
Primarily one needs to determine the cause of the goitre. This may be done by a biopsy using a fine needle. A thyroid scan may also be used, as well as ultrasound. Surgery aims to remove either part or the whole of the gland. If the entire gland is removed, you MUST take thyroid hormone replacement for the rest of your life.
Can it come back again?
Yes. This happens when surgery is done, leaving some of the gland behind. The remaining portion can grow again, but this is not common.
Is surgery for this condition dangerous?
A thyroid operation is major surgery. You must understand that any major operation can lead to complications. However, this is an operation that seldom leads to problems. One of the most common complications involves damage to a tiny nerve that controls the voice box (larynx). If this occurs, hoarseness, and a weak voice may result. Naturally, every effort is employed to prevent this happening.
What about after the operation?
After the operation you will have a cut which usually heals well. Placed at the lower part of the neck this is often difficult to see. If one is conscious about it, it can be concealed by a choker or similar bit of jewelry. Your stitches will be removed in about 4 days (if necessary). You may eat and drink normally.
Can I work after the operation?
Of course, after you have recovered, in about 3 to 4 weeks.
Can I function normally again?
Yes. If the entire gland is removed, you will need to take thyroxine tablets for the rest of your life. But this apart, life is normal.

What is a ganglion?
A ganglion cyst is one of a number of common, relatively harmless lumps that may form under the skin. These cysts typically form near or around joints, especially on the back of the hand and dorsum of the foot. They can be soft or quite tense and usually contain thick clear fluid very similar to joint fluid.
How did I get it?
These are degenerative cysts that form on their own. They are usually not related to any thing you've done.
Is it a dangerous condition?
No. They may be painful and unsightly when large, but not dangerous.
What will surgery do?
Remove the ganglion via a small incision in the skin under local anaesthesia.
Can it come back again?
Yes. Indeed, ganglions are notorious for returning again. Occasionally, they also disappear spontaneously.
Is surgery for this condition dangerous?
Ganglions occur in the vicinity of joints. In this location there are also nerves, tendons and blood vessels. Any of these may be injured, but with care and skill, this can usually be avoided. Even when some of these structures are damaged, no lasting harm may result. Tendons and nerves play important roles in movement and sensation respectively. Every care is taken not to damage these structures. A serious tendon injury may result in loss of function of a digit, while damage to a nerve may cause loss of sensation.
What about after the operation?
Pain may be prominent for a few days, but there are no serious after effects. Your stitches are usually removed in 7 to 10 days.
Can I work after the operation?
Yes. Depending on the kind of job you do, you may be fit to return to work in about 2 to 3 weeks.
Can I function normally again?
Yes. Removing a ganglion in no way incapacitates you, provided that important tendons and nerves are preserved.
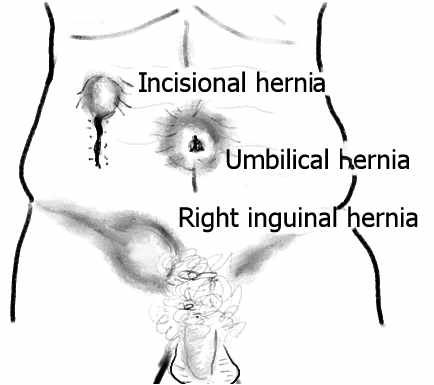
What is a hernia?
All hernias result from a weakness in some part of the body, which allows some other organ or part to bulge outward. Common sites for hernias are the groin (inguinal and femoral hernia), the navel (umbilical hernia), and the abdominal wall after an operation (incisional hernia). These weak areas are usually defects in an otherwise strong membrane called a sheath or fascia.
How did I get it?
You can be born with a hernia. This applies especially to males, who may be born with inguinal hernias. Umbilical hernias in both sexes are invariably present at birth, but usually correct themselves.
Alternatively, hernias can develop later in life for a number of reasons. The best example of this is an incisional hernia, which may occur after an abdominal operation if the wound has not healed properly. Sometimes a groin hernia will work its way into the scrotum, sometimes filling the entire scrotum with intestine.
Is it a dangerous condition?
While it is not uncommon for persons to keep a hernia for years without trouble, any hernia can lead to complications. The most dangerous of these is strangulation, where the blood supply to an organ or part of an organ (usually the intestine) trapped in the hernia, is cut off. This can be fatal. Prevention of this condition is the main reason for surgery.
What will surgery do?
In a nutshell, surgery will close the defect and attempt to strengthen the weak areas. There are two main techniques in use; one uses the body's natural tissues only, if they are in good shape; the other uses a special artificial cloth called "mesh" to provide strength to the weakened area that permits the hernia.
Can it come back again?
To be frank, yes! Many techniques exist for strengthening hernial areas. However, even in the best centres, a hernia may recur after surgery, especially if post-operative instructions are not adhered to. You must carefully follow instructions not to engage in heavy or strenuous activity for the period stipulated.
Is surgery for this condition dangerous?
Usually not. The operation lasts 30 minutess to 1 hour, and is well tolerated by any fit person. If there are pre-existing medical problems these may make any surgery more demanding and difficult. You should be aware however, that any operation may result in unexpected complications. Because of this, anyone having a general anaesthetic needs at a minimum a full medical examination, and a recent hemoglobin estimation (blood test).
What about after the operation?
Usually you will be allowed home a few hours after surgery, unless there are other concerns. You should get plenty of rest. It is important to observer the following:
- Do not engage in heavy manual labour. (Even vigorous straining at stool may be detrimental in the early stages.)
- Eat a normal diet.
- Remember to keep your appointment for removal of stitches, if so instructed.
- Do not tamper with the dressing. If you are worried about it, call.
- You may bathe normally, taking care to protect the dressing.
Can I work after the operation?
Yes. You will usually be advised to refrain from heavy activity for a period of 4 to 6 weeks. After this, you may usually return to full normal activity.
Can I function normally again?
Yes. A hernia operation does not permanently impair any bodily function.

What is laparoscopic cholecystectomy?
Cholecystectomy is the removal of the gallbladder. This may be done by opening the abdomen using an incision about 4 to 8 inches long and operating directly on the gallbladder. This was the standard method for many years.
A New Approach
In recent times, surgeons have been striving for "minimally invasive surgery" in which surgery is performed using a laparoscope, a slender instrument which can be introduced via small nicks in the abdomen. Laparoscopic chole-cystectomy removes the gallbladder using the laparoscope.
Where is my gallbladder?
The gallbladder is located just under the liver in the right upper section of the abdomen, under the rib cage. In health, provided you are not fasting, it is quite a small organ about the size of a large thumb.
Why do I need surgery?
The reasons are the same as for standard cholecystectomy - stones in the gallbladder. Sometimes the gallbladder becomes infected, again usually because of stones.
Is the condition dangerous?
Gallstones are very common, especially in females, usually over the age of thirty. Many persons have gallstones and never have any difficulty whatever. However, gallstones can cause pain in the abdomen, vomiting, and upset stomach. In acute cholecystitis, the gallbladder becomes infected, with the development of fever and severe abdominal pain. In rare cases perforation of the organ may occur, and may be life-threatening.
What will surgery do?
Under general anaesthesia, carbon dioxide gas is introduced into the abdomen to distend it. The laparoscope, with an electronic camera attached, is then inserted. This projects a clear image of the abdominal cavity onto a TV monitor. The surgeon then makes about three more tiny holes, and via these, various operating instruments are used to carefully dissect and remove the gallbladder. At the end of the surgery, the gas is removed and the tiny nicks closed.
Can the gallstones come back again?
Stones normally form in the gallbladder. Once this is removed, you will not form any more gallstones. However very rarely stones may be overlooked at the time of surgery in the common bile duct. Provided that these are discovered in time removal can often be done without a major operation, by a procedure called ERCP - Endoscopic Retrograde Cholangio-Pancreatography.
Is laparoscopic surgery for this condition dangerous?
Even though many persons are well enough to be back home in 24 hours, laparoscopic surgery is major surgery nevertheless, and has all the attendant risks that major surgery carries, such as infection, bleeding from the site of the surgery, pneumonia, thrombosis of the deep veins, etc.<p>
Use of the laparoscope carries with it other risks as well. The large abdominal vessels, or the gut itself may rarely be damaged while attempting to insert the various instruments. Complications caused by the carbon dioxide have also be known to occur. These are all rather uncommon, but are more likely in the person who has had abdominal surgery before.
What about after the operation?
You are usually well enough to return home within 24 hours. Mild soreness may be felt in the shoulder tips for a day or so - this results from small amounts of gas left in the abdomen.
Can I work again after this operation?
Most persons can be back to work within a week or less.
Will I function normally again?
Absolutely. Loss of the gallbladder in no way affects your normal lifestyle or eating habits.

What is a skin lump?
A number of common harmless lumps may form in or under the skin. These may occur in any location. These consist of a variety of conditions, notably cysts, especially epidermal cysts, lipomas (fatty lumps), fibromas (lumps of fibrous tissue), neuromas (nerve tissue), enlarged lymph nodes, and many others. Very uncommonly a lump may be cancerous. Recent rapid growth and pain in a lump especially should cause concern, but in the main infection will be the cause rather than cancer.
How did I get it?
These usually form on their own. Cysts may form when ducts (their openings) become blocked. Some lumps can be congenital (present from birth). Other lumps, like lymph nodes, may indicate the presence of other disease processes.
Are these dangerous conditions?
Usually not. They may be painful, and unsightly, but not dangerous. Rarely cancer of the skin may exist in the form of a lump, in which case it can be a very serious condition depending on its nature.
What will surgery do?
Remove the lump via a small incision in the skin and submit it for pathological examination. This ensures that a firm diagnosis is made and that the lump is removed.
Can it come back again?
Yes. A skin lump may form at any time. Some conditions are notorious for recurring if not completely removed. Your surgeon will alert you if there are any special instructions.
Is surgery for this condition dangerous?
Usually not. These lumps, if small will be removed under local anaesthesia (in the adult). If very large, then you may be put to sleep. Remember, any general anaesthetic may lead to complications.
What about after the operation?
Pain may be prominent for a few days, but there are no serious after effects. Your stitches are usually removed in 5 to 10 days depending on location.
Can I work after the operation?
Yes. Depending on the kind of job you do, an the location of the surgery, you may be fit to return to work in about 1 to 3 weeks.
Can I function normally again?
Yes. Removing a skin lump no way incapacitates you. The exceptions to this would be in cases where the lump revealed other more serious conditions needing further management.
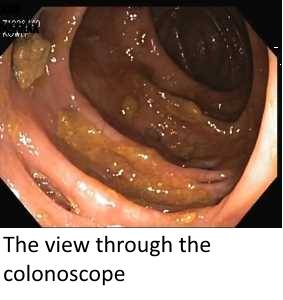
What is colonoscopy?
This is inspection of the large bowel with an instrument called a COLONOSCOPE.
It is one of a few methods to inspect the large bowel for various ailments, especially the presence of polyps and tumours and diverticular disease. It can also detect other less common disorders like inflammatory bowel disease, colitis etc.
The Colonoscope
This is a sophisticated optical tube which is flexible so that it can be manipulated through the normal twists and turns of the bowel. The procedure is often video-assisted, in which the picture of the bowel is viewed on a television screen for better comfort. The entire procedure can also be video-taped for discussion and review later.
Why do I need colonoscopy?
Colonoscopy is most often performed for problems of the large bowel - usually bleeding, pain on passing stool, constipation or diarrhoea. However unlike past methods, it allows the doctor to see much more of the large bowel, and in many cases almost the entire length of the gut can be clearly seen. Any unusual lumps or areas can also be biopsied. In this procedure small portions are removed and sent to the lab for pathological study. The following are views of normal bowel (with some yellow stool residue), polyps, cancer and diverticular disease seen with the colonoscope.
Are these conditions serious?
A surprisingly large number of persons suffer with trivial anal problems, especially piles (hemorrhoids), and small tears in the lower anus called fissures. Both of these may cause bleeding, pain and other difficulties in the toilet. However, bleeding and constipation may also signal more serious disease, notably cancer of the colon, or other growths in the bowel, both of which are potentially serious. Small polyps like that shown above can be removed with the colonoscope without the need for major surgery.
What happens at colonoscopy?
Prior to arriving for the procedure you will have been put on some sort of medication to clear out all the stool from the large gut, since solid stool renders the delicate instrument useless. You are then placed on your side on the operation table and the instrument is passed into the rectum, commonly with the assistance of mild sedation. A slight urge to go to the toilet is all you usually feel. During the procedure, air is forced into the bowel to distend it so that a clear view can be had. This makes you feel a bit bloated. You should report at once any significant pain.
As mentioned above, if any unusual areas or lumps are seen, they are biopsied. Occasionally small lumps called polyps can be completely removed during colonoscopy. These used to require major surgery for their removal in the past, but provided that they are not too big can now be treated by the colonoscope.
Is this procedure dangerous?
Examination with the flexible colonoscope is now safer than with the older rigid metal instruments. However, there are still risks attached. The main one is a perforation of the bowel. Especially when the gut is affected by disease of some sort, it can be penetrated by the colonoscope. This is a very major complication. Immediate admission to hospital (and often surgery) is a MUST in order to contain the damage and safeguard life. In some cases you may need to have a temporary colostomy for safety. In some situations, even the introduction of air into the bowel can result in perforation. Mild bleeding will usually be seen in the stool for about 24 hours if a biopsy has been done. Very rarely this bleeding may become significant and require further intervention.
What about after the operation?
Provided that all has gone well (which is the norm), you will be completely well after. The only discomfort relates to the passage of the air which was introduced as part of the colonoscopy.
Can I work again after this operation?
Certainly - usually on the next day.
Will I function normally again?
Generally yes. Simply having a colonoscopy in no way impairs any bodily functions.

Hemorrhoids
...or piles as they are more commonly known are one of mankind's most common maladies. If three people pass you on the street, at least one is likely to have, or have had, some trouble with piles.
So what are piles?
Piles are simply enlarged blood vessels, no more, no less. The rectum and anus are richly supplied with blood vessels, as are many orifices in the body. There are many theories to explain why they become problematic, but the short story is that these blood vessels enlarge and become swollen over time. They can get so big that they prolapse (are forced out the anus) during straining at stool. Some eversion of the anus (turning out of the mucosa) is normal during stooling but piles represent a significant distortion of this mechanism.
When this happens, if the swelling does not return or if it is not replaced (more on this later), significant pain with or without bleeding can occur. It is this pain and bleeding that brings people to the doctor.
What causes piles?
As with so many things in life, there are many causes, but the two that usually stand out are:
- diet poor in fibre
- constipation and straining

Fibre
In the good old days when we lived in caves and ate naturally, food was high in fibre content. Fibre is the crunchy non-digestible component of many plant foods like the pith in citrus, the leafy parts of cabbage, the crunchy parts of carrots. Fibre is also a significant part of root crops like sweet potato and cassava. It is also abundant in the grains of corn and wheat, as well as peas, beans etc. Indeed, fibre is widely found in nature.
But then we came out of the cave, built homes and processed our food. Wives prefer soft white flour, so manufacturers removed the fibre. We prefer processed orange juice rather than the natural fruit with all that messy pith to chew. And when we now cook, we usually cook the hell out of food. Over-cooking will degrade fibre which structurally is a long carbohydrate chain. Too much cooking breaks these chains apart and degrades the fibre. Add to this the fact that many people just hate fruits and vegetables and you have a situation where lots of us simply don't get enough fibre in our daily diet.
What is the good of having fibre in our diet?

Stool is a complex, albeit smelly, material consisting of undigested food elements, dead gut cells, bacteria and various unfriendly chemicals that are best gotten rid of. A significant part of stool is its water content. The more water stool contains, up to a point, the softer it is and the more easily it is passed.
Stool gets harder and harder the longer it stays in the rectum. Many people for various reasons - work, busy schedules, old habits etc, tend to put off going to the toilet when they feel the urge. Several litres of gut contents enter the large bowel on a daily basis. One important function of the large gut is to return most of this water to the body. If this fails, massive, life threatening diarrhoea results. However if stool stays parked in the large bowel for too long, more and more water gets extracted and soon the stool is rock hard. This results in constipation.
What fibre does is quite important. It is not digested and so stays in the stool as it passes through the gut. Because of its chemical structure, fibre attracts and holds water in its physical structure. Since water stays with fibre and fibre stays with the stool, the latter tends to remain soft and pliable the more fibre it contains. So a good daily helping of fibre is critical for well formed, soft stool. Little or no fibre means that stool becomes cannon balls. When this happens, we strain and force. It is this straining and forcing that over time causes piles to develop. At least so the theory goes. However many people with piles deny any constipation.

Is surgery for piles painful?
In the majority of times, piles can be managed without any surgery at all. Given the causes mentioned above, treatment of piles usually involves the following:
- changing the diet to include fibre
- as well as more fluid
- avoidance of constipation and straining
- including exercise in one's daily regime
- promply replacing any piles that prolapse
Even when piles are present, if they remain inside the rectum, they cause little discomfort even when they bleed. It is when they prolapse and become swollen and engorged that pain becomes significant. The remedy for this is simple, though not necessarily easy or comfortable. All that is required is to push them back. Early in the disease process, this is fairly easy. All one has to do is lubricate the first two fingers (use a water based jelly rather than vaseline which is oil based), and apply gentle pressure on the swelling while lying down and relaxing the anus. With practice, the swelling can be gently pushed back in.
Much later in the disease, when the mass can reach tremendous size, this may not be possible even with medical expertise in the office. In such cases, it may require hospitalization and replacement under anaesthesia. It is only if prolapse happens repeatedly and causes significant and unrelenting discomfort, that surgery of some sort is needed.
But surery doesn't always mean cutting.
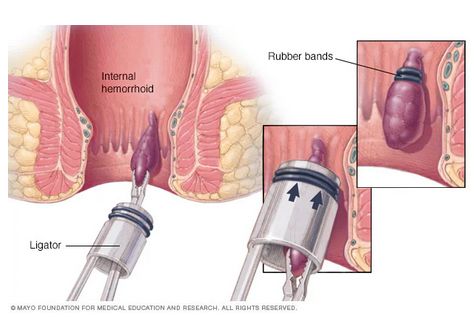
Rubber band treatment
Fairly simple, usually solitary piles can be "strangulated" by placing a tight rubber band around the base. This cuts off the blood supply and the swelling dries up and falls away in a week or so. The same thing can be achieved by surgically tying a suture around the base. Usually when a suture is used, the surgeon will simply cut the hemorrhoid off at the same time.
However some hemorrhoids are huge, complex and involve the entire circumference of the anus. In such cases, extensive surgery may be required where all the affected tissue is cut away and the anus reconstructed. Such cases can result in significant postpoperative pain and discomfort, especially at the first stool after surgery. Luckily these cases are in the minority.
The main lesson from all this is:
- get plenty of fibre in your daily diet
- avoid highly processed foods as much as possible
- try to obey the urge to stool whenever possible
- drink plenty of fluids daily (doesn't have to be water)
- don't get constipated
- don't strain at stool
- exercise
Do all this, and your anus will love you. On the other hand, making an enemy of your anus doesn't pay. You will lose the war, every time. Piles will see to that.
Constipation
Constipation refers to:
- hard stool
- infrequent stooling (eg once a week)
- both hard and infrequent stools
Almost everybody at some time in their lives may suffer a bout of constipation, often due to a change of diet, travel to unfamiliar destinations, illness or surgery. Stools become rock hard and may cause pain and bleeding. Constipation also occurs when stooling is very infrequent, sometimes not happening for weeks.
Constipation is so closely allied to hemorrhoids (piles) that you are being directed to that topic for a continuation of the subject. Click here to continue.
